Educational Overview of IVF – Options for Older Women
- Alifiya Batterywala
- Jan 29
- 8 min read
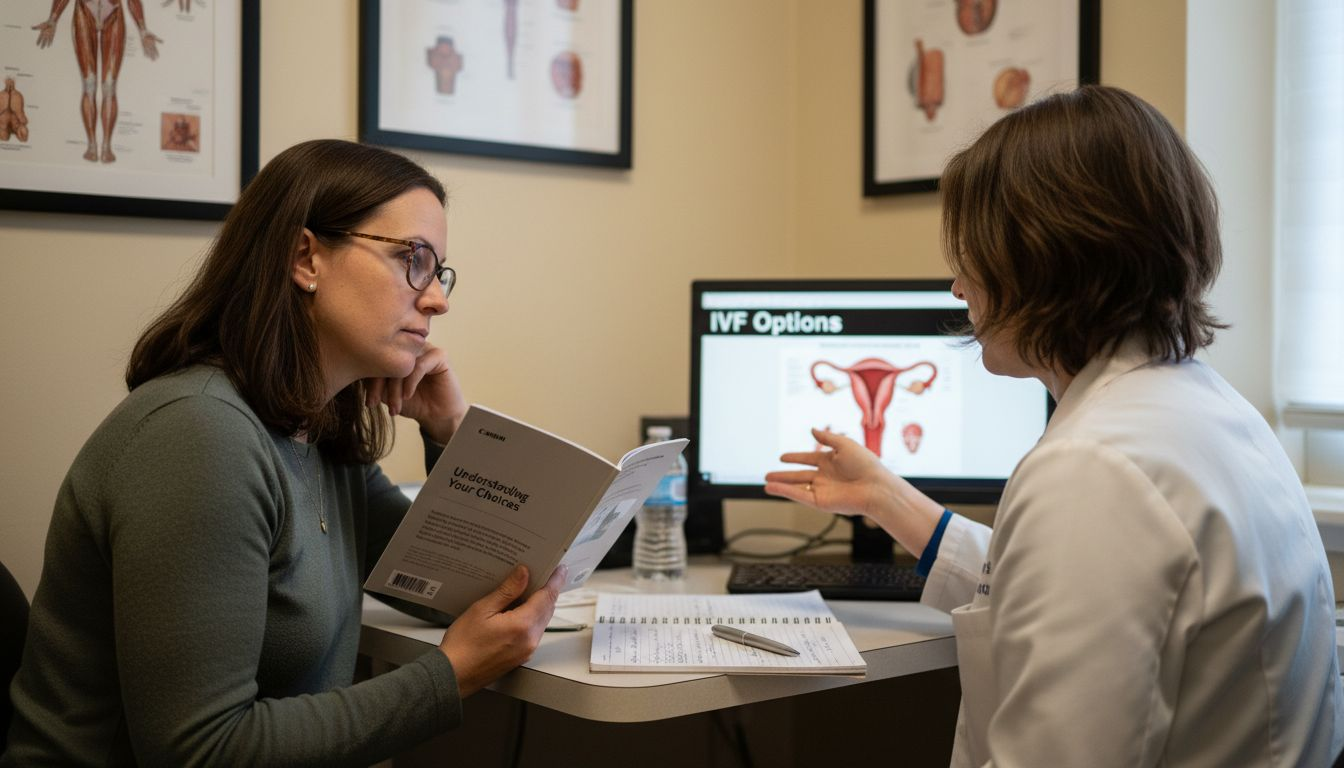
Facing fertility challenges after 40 can feel daunting, especially when diminished ovarian reserve or genetic concerns add uncertainty. For many women, IVF represents hope and possibility, with assisted reproductive technology helping millions worldwide build families over the past four decades. At a leading Bahamas clinic, advanced techniques and personalized care empower women to pursue parenthood with confidence, focusing on optimizing egg quality and tailoring every step to unique reproductive needs.
Table of Contents
Key Takeaways
Point | Details |
IVF Overview | IVF is a complex procedure combining egg retrieval, fertilization, and embryo transfer to assist individuals with fertility challenges. It has successfully helped many people achieve parenthood over the last four decades. |
Types of IVF | Various IVF methods exist, such as Natural Cycle IVF and ICSI, allowing for tailored approaches based on individual medical histories and fertility issues. |
Considerations for Women Over 40 | Increased age may impact egg quality and fertility; personalized protocols and advanced techniques can improve outcomes. |
Financial and Emotional Planning | Understanding costs and securing emotional support are crucial for navigating the IVF process effectively. |
What Is IVF and How Does It Work
In vitro fertilization (IVF) is an advanced reproductive technology designed to help individuals and couples struggling with fertility challenges. This complex medical procedure involves retrieving eggs from a woman’s ovaries and manually fertilizing them with sperm in a specialized laboratory setting. Assisted reproductive technologies like IVF have successfully helped millions of people become parents over the past four decades.
The IVF process follows a carefully structured sequence of medical interventions:
Ovarian stimulation using hormonal medications
Egg retrieval through minimally invasive procedures
Sperm collection and laboratory preparation
Fertilization and embryo development
Embryo transfer into the uterus
Pregnancy testing and monitoring
For women over 40, IVF becomes particularly nuanced due to age-related fertility challenges. The procedure addresses multiple reproductive obstacles, including:
Blocked or damaged fallopian tubes
Reduced ovarian reserve
Diminished egg quality
Male factor infertility
Unexplained fertility issues
Egg Quality is a critical factor in IVF success for older women. As women age, their egg quantity and genetic integrity naturally decline, which can impact fertilization rates and embryo development. Advanced IVF techniques now incorporate sophisticated screening methods to improve outcomes.
Success Rates vary significantly based on individual factors. While younger patients experience higher pregnancy rates, modern reproductive technologies continue expanding possibilities for women in their late 30s and 40s.
Pro Tip: Consider comprehensive genetic screening and consulting a fertility specialist who specializes in advanced reproductive techniques for women over 40.
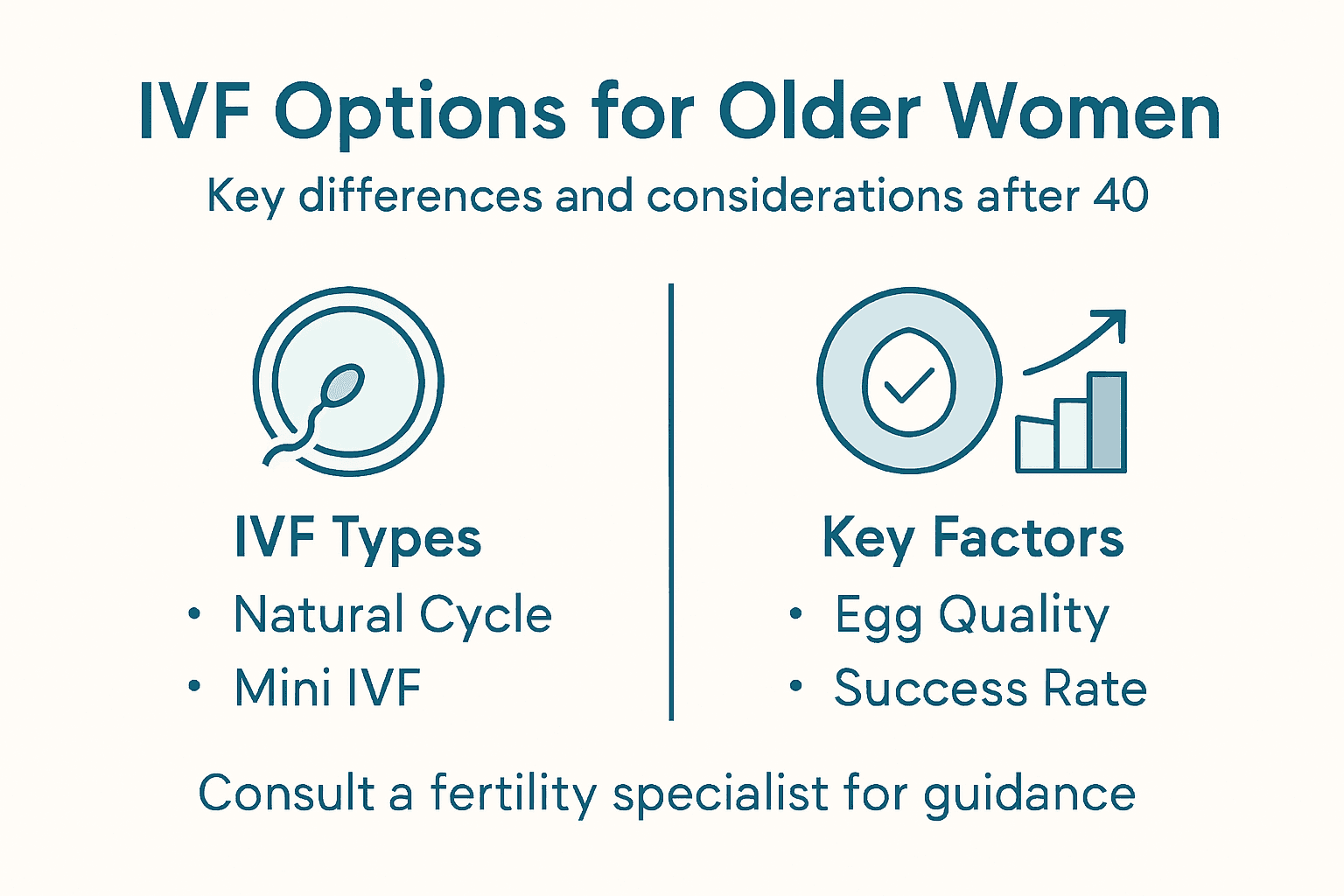
Types of IVF and Key Differences
In the realm of fertility treatments, multiple IVF approaches exist to address specific reproductive challenges for women over 40. Fertility science continues advancing options for patients with complex reproductive needs, offering increasingly specialized techniques.
The primary types of IVF procedures include:
Natural Cycle IVF: Minimally invasive approach using a woman’s natural monthly cycle
Mild/Mini Stimulation IVF: Uses lower hormone doses to produce fewer eggs
Traditional Full Stimulation IVF: Maximum hormone stimulation to produce multiple eggs
Frozen Embryo Transfer (FET): Involves transferring previously frozen embryos
Intracytoplasmic Sperm Injection (ICSI): Specialized fertilization technique for male factor infertility
Age-Related Considerations play a crucial role in selecting the most appropriate IVF approach. Women over 40 often require more personalized protocols due to reduced ovarian reserve and egg quality. Each technique offers unique advantages depending on individual medical history, fertility challenges, and reproductive goals.
Key differentiating factors among IVF types include:
Here’s a comparison of major IVF types and when they are often recommended:
IVF Approach | Typical Candidate | Medication Intensity | Unique Advantage |
Natural Cycle IVF | Women with regular cycles | Minimal | Low risk, no ovarian stimulation |
Mild/Mini Stimulation IVF | Those seeking milder side effects | Moderate | Fewer eggs, reduced discomfort |
Traditional Full Stimulation IVF | Most patients, low reserve | High | Maximizes egg retrieval |
Frozen Embryo Transfer (FET) | Previous IVF, egg freezing | Depends on protocol | Flexible timing, preserves embryos |
ICSI | Male factor infertility | Combined with any IVF | Assists fertilization with poor sperm |
Medication protocols
Number of eggs retrieved
Stimulation intensity
Embryo selection methods
Genetic screening options
Cost and insurance coverage
Success Rates vary significantly across different IVF approaches. Factors like egg quality, sperm parameters, and underlying reproductive health dramatically influence outcomes. Advanced IVF innovations continue expanding possibilities for women facing complex fertility challenges.
Pro Tip: Consult a reproductive specialist who can perform comprehensive diagnostic testing to determine the most suitable IVF approach for your specific fertility profile.
Step-By-Step IVF Process Explained
The IVF journey is a meticulously planned medical procedure designed to maximize reproductive potential for women facing fertility challenges. IVF procedures involve complex laboratory techniques that transform reproductive possibilities for patients over 40.
The comprehensive IVF process typically unfolds through these critical stages:
Initial Consultation and Testing
Comprehensive medical history review
Fertility diagnostic testing
Genetic screening
Ovarian reserve assessment
Ovarian Stimulation
Hormone medications administered
Regular ultrasound monitoring
Tracking follicle development
Preventing premature ovulation
Egg Retrieval
Minor surgical procedure
Performed under mild anesthesia
Ultrasound-guided needle aspiration
Collecting mature eggs
Fertilization
Combining eggs with sperm
Potential intracytoplasmic sperm injection (ICSI)
Monitoring fertilization progress
Embryo culture
Embryo Transfer
Selecting highest quality embryos
Precise uterine placement
Optional genetic screening
Potential multiple embryo transfer
Hormone Support plays a crucial role throughout the IVF process. Women over 40 often require additional hormonal interventions to support potential embryo implantation and early pregnancy development. Advanced fertility treatments continue expanding success rates for patients with complex reproductive histories.
Key considerations for women over 40 include egg quality, potential genetic screening, and individualized treatment protocols. Each stage requires careful medical supervision and personalized approach to maximize potential success.
Pro Tip: Maintain detailed medical documentation and communicate openly with your reproductive specialist to optimize your personalized IVF treatment strategy.
Advanced IVF Techniques for Low Ovarian Reserve
Women with diminished ovarian reserve face complex fertility challenges that require specialized reproductive strategies. Management of low ovarian response demands innovative approaches tailored to individual reproductive profiles.
Key advanced techniques for addressing low ovarian reserve include:
Minimal Stimulation Protocols
Customized hormonal interventions
Reduced medication dosages
Personalized egg retrieval strategies
Specialized Stimulation Approaches offer promising alternatives for women with reduced egg production:
Micro-Dose Gonadotropin Protocols
Ultra-low hormone stimulation
Minimizes potential ovarian stress
Targets quality over quantity
Growth Hormone Adjuvants
Supplemental hormonal support
Potential improvement in egg quality
Enhanced follicular development
Natural Cycle IVF
Minimal pharmaceutical intervention
Works with single naturally occurring egg
Reduces physiological stress
Emerging Technologies continue expanding reproductive possibilities. Advanced fertility options now include cutting-edge techniques like mitochondrial replacement and stem cell therapies that could potentially regenerate ovarian function.
Comprehensive genetic screening and personalized treatment plans are crucial for women with low ovarian reserve. Each approach must be meticulously customized to individual physiological characteristics and reproductive goals.
Pro Tip: Consult a reproductive specialist who specializes in advanced techniques for women with diminished ovarian reserve to develop a comprehensive, personalized fertility strategy.
Costs, Risks, and Common Misconceptions
Navigating the complex landscape of IVF requires understanding potential medical, financial, and emotional considerations. IVF safety protocols have significantly improved patient outcomes and minimized historical risks associated with reproductive technologies.
Medical Risks associated with IVF include:
Ovarian hyperstimulation syndrome (OHSS)
Potential medication side effects
Minor surgical risks during egg retrieval
Increased probability of multiple pregnancies
Potential hormonal fluctuations
Financial Considerations vary dramatically across different reproductive centers:
Below is a summary of major IVF cost factors and patient considerations:
Cost Component | Typical Range | Impact on Patients |
Base IVF Cycle Fee | $12,000–$25,000 | Can limit access, varies by clinic |
Genetic Screening Add-ons | $1,500–$5,000+ | Enhances outcomes, increases cost |
Medication Expenses | $2,000–$7,000 | Varies by protocol, affects total |
Insurance Coverage | Partial/None | Determines out-of-pocket need |
Average IVF cycle costs range from $12,000 to $25,000
Multiple cycle packages might offer discounted rates
Insurance coverage differs extensively between providers
Additional genetic screening increases overall expenses
Common Misconceptions about IVF often create unnecessary anxiety:
Myth: IVF always leads to multiple births
Myth: IVF increases cancer risks
Myth: IVF guarantees pregnancy
Myth: IVF babies are less healthy
Reproductive health research demonstrates that most IVF-conceived children are as healthy as naturally conceived children. The perception of increased risks often stems from misunderstanding complex medical processes.
While medical risks exist, modern reproductive technologies have dramatically improved safety standards and success rates for patients.
Emotional Preparedness is equally crucial. The IVF journey involves significant psychological components that require comprehensive support and realistic expectations.
Pro Tip: Create a comprehensive financial and emotional support plan before starting IVF, including potential insurance coverage, savings strategy, and mental health resources.
Alternative Fertility Options Beyond IVF
Fertility challenges demand a comprehensive approach that extends beyond traditional in vitro fertilization. Optimizing natural fertility involves exploring multiple strategic interventions tailored to individual reproductive health needs.
Alternative Fertility Treatment Options include:
Ovulation Induction Medications
Oral medications like Clomiphene
Injectable gonadotropins
Stimulates egg production
Lower cost alternative to IVF
Intrauterine Insemination (IUI)
Direct sperm placement into uterus
Minimally invasive procedure
Higher success rates for specific conditions
Less expensive than IVF
Third-Party Reproductive Strategies offer additional pathways:
Egg donation
Sperm donation
Gestational surrogacy
Embryo adoption
Fertility treatment research demonstrates that combination approaches often yield the most promising outcomes. Women over 40 might benefit from integrating multiple strategies.
Comprehensive fertility care requires personalized medical assessment and a multi-dimensional treatment approach.
Surgical Interventions can address specific reproductive obstacles:
Correcting anatomical abnormalities
Removing fibroids or endometriosis
Unblocking fallopian tubes
Addressing hormonal imbalances
Pro Tip: Schedule comprehensive diagnostic testing to understand your unique fertility profile and develop a targeted, multi-strategy reproductive plan.
Empower Your Fertility Journey with Advanced IVF Solutions at Rejuvenating Fertility Center
Facing fertility challenges over 40 can be daunting. This article highlights critical issues such as diminished ovarian reserve, reduced egg quality, and the need for personalized IVF protocols to improve chances of success. At Rejuvenating Fertility Center in The Bahamas, we specialize in cutting-edge treatments like Mitochondrial Replacement Therapy and Stem Cell Therapy designed specifically for women dealing with low ovarian reserve or genetic concerns. Our approach offers hope where traditional methods may fall short by enhancing egg and embryo quality through innovative reproductive technologies.

Take control of your reproductive future today by exploring advanced IVF and ovarian rejuvenation options tailored to your unique needs. Visit Rejuvenating Fertility Center to learn more about our personalized care and breakthrough treatments. Discuss your fertility goals with Dr. Zaher Merhi and his expert team to develop a strategy that aligns with your journey. Don’t wait to find out how modern IVF innovations can open new possibilities — start your consultation now at https://rfcbahamas.com.
Frequently Asked Questions
What is IVF and how does it work?
In vitro fertilization (IVF) is a reproductive technology that involves retrieving eggs from a woman’s ovaries and fertilizing them with sperm in a lab. The process includes ovarian stimulation, egg retrieval, fertilization, embryo development, and embryo transfer into the uterus.
What are the different types of IVF available for older women?
The main types of IVF for older women include Natural Cycle IVF, Mild/Mini Stimulation IVF, Traditional Full Stimulation IVF, Frozen Embryo Transfer (FET), and Intracytoplasmic Sperm Injection (ICSI). Each method caters to specific reproductive challenges and personal medical histories.
How does age affect IVF success rates for women over 40?
Age significantly influences IVF success rates. Women over 40 generally face challenges with reduced egg quality and quantity. Advanced technologies are improving outcomes, but success rates remain higher for younger patients compared to those in their late 30s and 40s.
What are the risks and costs associated with IVF treatments?
The risks of IVF include ovarian hyperstimulation syndrome (OHSS) and potential surgery-related complications, among others. Financially, IVF costs can range from $12,000 to $25,000 per cycle, with additional expenses for medication and genetic screening. Insurance coverage may vary widely, impacting overall costs.
Recommended
Comments